-
- Федеральное государственное бюджетное образовательное учреждение высшего образования «Саратовский государственный медицинский университет имени В. И. Разумовского» Министерства здравоохранения Российской Федерации (410012, г. Саратов, Россия)
Ключевые слова: М2-пируваткина, матриксные металлопротеиназы (ММП), кальпротектин, лактоферрин, антинейтрофильные цитоплазматические антитела (ANCA), анти-Saccharomyces cerevisae антитела (ASCA)
Резюме: Распространенность воспалительных заболеваний кишечника (ВЗК) (язвенного колита (ЯК) и болезни Крона (БК)) ежегодно увеличивается. Актуальными остаются проблемы ранней и неинвазивной диагностики ВЗК. Цель настоящего обзора — анализ диагностической ценности различных биологических маркеров ВЗК. Основная цель поиска новых биомаркеров ВЗК заключена в возможности минимизировать повторные эндоскопические исследования для ранней диагностики и определения активности заболевания, оценки эффективности лечения и профилактики осложнений. Представлены широко используемые, рутинные, а также перспективные биологические маркеры, позволяющие верифицировать диагноз ВЗК, оценить течение и прогноз болезни.
-
- Belousova E.A. Epidemiology of inflammatory bowel disease in Russia. Falk Symposium. 2006: 31.
- Magro F., Gionchetti P.P., Eliakim R. et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Journal of Crohn's & Colitis. 2017; 11(6): 650. doi: 10.1093 / ecco-jcc / jjx008.
- Silverberg M.S., Satsangi J., Ahmad T. et al. Toward an integrated clinical, molecular and serological classifшcaton of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterologists. Canadian journal of gastroenterology. 2005; 19:5-36. doi: 10.1155/2005/269076.
- Ивашкин В.Т., Шелыгин Ю.А., Халиф И.Л. и соавт. Клинические рекомендации российской гастроэнтерологической ассоциации и ассоциации колопроктологов России по диагностике и лечению болезни Крона. 2017:9-10.
- Reinink A.R., Lee T.C., Higgins P.D. Endoscopic mucosal healing predicts favorable clinical outcomes in infammatory bowel disease: a meta-analysis. Inflammatory bowel diseases. 2016; 22:1859-1869. doi: 10.1097/MIB.0000000000000816.
- Lennard-Jones J.E., Shivananda S. Clinical uniformity of inflammatory bowel disease a presentation and during the first year of disease in the north and south of Europe. EC-IBD Study Group. European journal of gastroenterology and hepatology. 1997;4:353-359.
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clinical Pharmacology & Therapeutics. 2001; 69(3): 89-95. doi: 10.1067/mcp.2001.113989.
- Mikhailova I.E., Philipenko N.V. Biomarkers of inflammatory bowel disease. Medical science. 2011; 4(20): 61-66.
- Михайлова И.Е., Филипенко Н.В. Биомаркеры воспалительных заболеваний кишечника. Лечебное дело. 2011; 4(20): 61-66.
- Yoon J.Y., Park S.J., Hong S.P. et al. Correlations of Creactive protein levels and erythrocyte sedimentation rates with endoscopic activity indices in patients with ulcerative colitis. Digestive Diseases and Sciences. 2014; 59(4): 829-837. doi: 10.1007/s10620-013-2907-3.
- Magro F., Gionchetti P.P., Eliakim R. et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Journal of Crohn's & Colitis, 2017; 11(6): 651. doi: 10.1093 / ecco-jcc / jjx008.
- Silberer H., Küppers B., Mickisch O. et al. Fecal leukocyte proteins in inflammatory bowel disease and irritable bowel syndrome. Clinical laboratory. 2005: 51(3-4): 117126. doi: 10.1186/1471-230X-14-121.
- Fischbach W., Becker W., Mössner J. et al. Leucocyte elastase in chronic inflammatory bowel diseases: a marker of inflammatory activity? Digestion.1987; 37:88-95.
- Langhorst J.В., Boone J., Lauche R. et al. Fecal lactoferrin, calprotectin, PMN-elastase, CRP, and white blood cell count as indicators for mucosal healing and clinical course of disease in patients with mild to moderate ulcerative colitis: post hoc analysis of a prospective clinical trial. Journal of Chron’s & colitis. 2016; 10(7): 786-794. doi: 10.1186/s12876-016-0462-z.
- Baker E.N., Baker H.M. Molecular structure, binding properties and dynamics of lactoferrin. Cell Molecular Life and Science. 2005; 62: 2531-2539. doi: 10.1007 / s00018-005-5368-9.
- Gartia-Montoya I.A., Cendón T.S., Arévalo-Gallegos S. et al. Lactoferrin a multiple bioactive protein: An overview. Biochemical Biophysycal Acta. 2012; 1820: 226-236. doi: 10.1016 / j.bbagen.2011.06.018.
- Troost F.J., Steijns J., Saris W.H., Brummer R.J. Gastric digestion of bovine lactoferrin in vivo in adults. Journal of Nutrition. 2001; 131(В): 2101-2104. doi: 10.1093/jn / 131.8.2101.
- Dai J., Liu W.Z., Zhao Y.P. et al. Relationship between fecal lactoferrin and inflammatory bowel disease. Scandinavian journal of gastroenterology. 2007; 42(12): 1440-1444. doi: 10.1080/00365520701427094.
- Fagerhol M.K., Dale I., Andersson T. A radioimmunoassay for a granulocyte protein as a marker in studies on the turnover of such cells. Bulletin Europeen de Physiopathologie Respiratoire. 1980; 16: 273–282.
- Roseth A.G., Schmidt PP.N., Fagerhol M.K. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scandinavian journal of gastroenterology. 1999; 34(1): 50-54.
- Walsham N.E., Sherwood R.A. Fecal calprotectin in inflammatory bowel disease. Clinical and experimental gastroenterology. 2016; 9: 21-29. doi: 10.1155/2016/5423043.
- Lee Y.M., Lee K.M., Lee J.M. et al. The usefulness of fecal calprotectin in assessing inflammatory bowel disease activity. The Korean journal of internal medicine. 2018; 2016: 324. doi: 10.3904/kjim.2016.324.
- Kawashima K., Ishihara S., Yuki T. et al. Fecal calprotectin level correlated with both endoscopic severity and disease extent in ulcerative colitis. BMC gastroenterology. 2016; 0462:1-6. doi: 10.1186 / s12876-016-0462-З.
- Vogl, T. S100A12 is expressed exclusively by granulocytes and acts independently from MRP8 and MRP14. Journal of biological chemistry. 1999; 274: 25291–25296. doi: 10.1074/jbc.274.36.25291.
- Yang Z. Proinflammatory properties of the human S100 protein. Journal of leukocyte biology. 2001; 69: 986–994. doi: 10.1189/jlb.69.6.986.
- Foell D., Kucharzik T., Kraft M. et al. Neutrophil derived human S100A12 (EN-RAGE) is strongly expressed during chronic active inflammatory bowel disease. Gut. 2003; 52(6): 847-853. doi: 10.1136/gut.52.6.847.
- Solovieva N.I. Matrix metalloproteinases and their biological functions. Bioorganic chemistry. 1998; 24(4): 245-255.
- Visse R., Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circulation research. 2003; 92(8): 827—839. doi: 10.1161/01.RES.0000070112.80711.3 D.
- Vu T.H., Werb Z. Matrix metalloproteinases: effectors of development and normal physiology. Genes & development. 2000; 14: 2123-2133. doi: 10.1101/ gad.815400.
- Ramnath N., Creaven PP.J. Matrix metalloproteinase inhibitors. Current oncology reports. 2004; 6(2): 96—102. doi: 10.1007/s11912-004-0020-7.
- von Lampe B., Barthel B., Coupland S.E. et al. Differential expression of matrix metalloproteinases and their tissue inhibitors in colon mucosa of patients with inflammatory bowel disease. Gut. 2000; 47(1): 63–73. doi: 10.1136/ gut.47.1.63.
- Faubion W.A. Jr., Fletcher J.G., O'Byrne S. et al. Emerging BiomARKers in Inflammatory Bowel Disease (EMBARK) study identifies fecal calprotectin, serum MMP9, and serum IL-22 as a novel combination of biomarkers for Crohn’s disease activity: role of cross-sectional imaging. American journal of gastroenterology. 2014; 109(5): 780. doi: 10.1038/ajg.2013.354.
- Jakubowska K., Pryczynicz A., Iwanowicz P. et al. Expression of matrix metalloproteinases (MMP2, MMP-7, and MMP-9) and their inhibitors (TIMP-1, TIMP-2) in inflammatory bowel diseases. Gastroenterology research and practice. 2016; 2016: 1-7. doi: 10.1155/2016/2456179.
- Козлова И.В., Осадчук М.А., Кветной И.М., Попучиев В.В. Апудоциты и тучные клетки при хронических воспалительных заболеваниях толстой Тер. архив. 2000; 72(2): 32-35.
- Yamamoto T., Shira bbki M., Bamba T. et al. Fecal calprotectin and lactoferrin as predictors of relapse in patients with quiescent ulcerative colitis during maintenance therapy. International journal of colorectal disease. 2014; 29(4): 485-491. doi: 10.1007/s00384-0131817-3.
- Yamamoto T., Shiraki M., Bamba T. et al. Faecal calprotectin and lactoferrin as markers for monitoring disease activity and predicting clinical recurrence in patients with Crohn's disease after ileocolonic resection: A prospective pilot study. United European gastroenterology journal. 2013; 1(5): 368-374. doi: 10.1177/2050640613501818.
- Burmester G.R., Pecutto A., Ulrikhs T., Ayher A. Visual immunology. Laboratory of scince. Trans. from eng. 2018; 308 с.
- Czaja A.J., Shums Z., Donaldson P.T., Norman G.L. Frequency and significance of antibodies to Saccharomyces cerevisiae in autoimmune hepatitis. Digestive Diseases and Sciences. 2004; 49(4): 611-618. doi: 10.1023/B:DDAS.0000026306.36511.c8.
- Hardt PP.D., Toepler M., Ngoumou B. et al. Measurement of fecal pyruvate kinase type M2 (tumor M2-PK) concentrations in patients with gastric cancer, colorectal cancer, colorectal adenomas and controls. Anticancer Research. 2003; 23(2A): 851-853.
- Goonetilleke K.S., Mason J.., Siriwardana P. et al. Diagnostic and prognostic value of plasma tumor M2 pyruvate kinase in periampullary cancer: evidence for a novel biological marker of adverse prognosis. Pancreas. 2007; 34(3): 318-324. doi: 10.1097 / MPA.0b013e31802ee9c7.
- Li Y., Wang J.J. Clinical significance of blood and fecal tumor M2-pyruvate kinase expression in patients with colorectal cancer. Nan fang Yi Ke da xue xue bao. 2011; 31(12): 2087-2089.
- Vazquez Moron J., Pallarés Manrique H., Machancoses F.H. et al. Accurate cut-offs for predicting endoscopic activity and mucosal healing in Crohn's disease with fecal calprotectin. Revista espanola de enfermedades degistivas. 2017; 109(2): 130-136. doi: 10.17235 / reed.2017.4542/2016.
- Meng W., Zhu H.H., Xu Z.F. Serum M2-pyruvate kinase: A promising non-invasive biomarker for colorectal cancer mass screening. World journal of gastrointestinal oncology. 2012; 4(6): 145-151. doi: 10.4251/wjgo.v4.i6.145.
- Kozlova I.V., Osadchuk M.A., Kvetnoy I.M. et al. Melatonin and serotonin in inflammatory bowel diseases and colorectal cancer. Clin. Med. 2000;6: 32-35.
- Rath T., Roderfeld M., Graf J. et al. Enhanced expression of MMP-7 and MMP-13 in inflammatory bowel disease: a precancerous potential? Inflammatory bowel diseases. 2006; 12(11): 1025–1035. doi: 10.1097/01. mib.0000234133.97594.04.
Для цитирования :
Козлова И. В., Кудишина М. М., Пахомова А. Л. Биомаркеры воспалительных заболеваний кишечника. Экспериментальная и клиническая гастроэнтерология. 2018;157(9): 4–9. DOI: 10.31146/1682-8658-ecg-157-9-4-9.
Загрузить полный текст
ОГЛАВЛЕНИЯ ВЫПУСКОВ
Контакты
Submission of the manuscript is online via e-mail
ecgarticle@gmail.com or
cholerez@mail.ru
Editorial Correspondence e-mail
gastrossr@gmail.com
Publishing, Subscriptions, Sales and Advertising, Correspondence e-mail
journal@cniig.ru
Tel: +7 917 561 9505
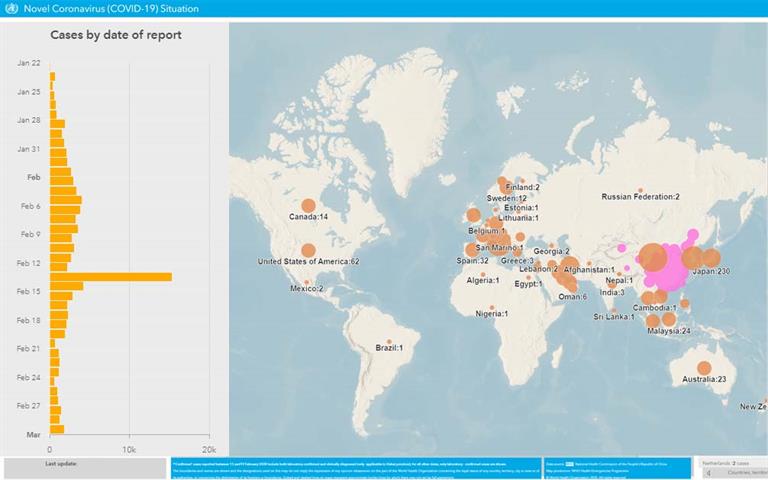
COVID-19