-
- ФГБУ «ГНЦК им. А.Н. Рыжих» Минздрава России, 123423 Москва, Россия, ул. Саляма Адиля, 2
- Факультет повышения квалификации медицинских работников Российский университет дружбы народов, 117198, г. Москва, ул. Миклухо-Маклая, д. 21, корпус 3
- ГБУЗ городская поликлиника № 218 ДЗМ, филиал № 3 в Лосиноостровском районе, 1-я Напрудная улица, 15
- ФГБОУ ДПО РМАНПО Минздрава России, 125993, г. Москва, Россия, ул. Баррикадная, д. 2⁄1, стр. 1
Ключевые слова: Clostridium (Clostridioides) diffi cile, C. diffi cile-ассоциированная инфекция, антибиотикорезистентность, механизмы резистентности к антибактериальным препаратам.
Резюме:Цель. Изучить и объединить в одном обзоре современные данные о механизмах антибактериальной резистентности Clostridium (Clostridioides) diffi cile. Существуют объективные данные о распространении резистентных к антибактериальным препаратам штаммов Clostridium (Clostridioides) diffi cile. Описаны механизмы резистентности бактерии, которые детерминируются генами резистентности, содержащимися в бактериальной хромосоме и/или метаболических путях. Распространение резистентности среди клинических штаммов С. diffi cile усугубляется способностью бактерий образовывать биопленки. Кроме того, являясь спорообразующей бактерией, C. diffi cile в споровой форме способна выдерживать действие антибактериальных препаратов, а после прекращения антибактериальной терапии переходить в вегетативную форму, тем самым вызывая рецидив заболевания. Понимание механизмов резистентности C. diffi cile один из ключевых моментов в стратегии предотвращения развития заболевания. Помимо рационального использования антимикробных препартов, необходим мониторинг распространения резистентности среди C. diffi cile. По нашему мнению, необходимо продолжать исследования, направленные на изучение механизмов резистентности к антибактериальным препаратам у C. diffi cile и разработку новых противомикробных средств, эффективных против этого патогена.
-
- Муляр, Н. Ф., Верещагина, С. А., Фадеева, Т. В. и соавт. Clostridium diffi cile-ассоциированные диареи в многопрофильном стационаре //Бюллетень Восточно-Сибирского научного центра Сибирского отделения Российской академии медицинских наук. – 2012. – № 5–1 (87). – 72–75.
- Дмитриева Н. В., Клясова Г. А., Бакулина Н. В., и соавт. Распространенность Clostridium diffi cile-ассоциированной диареи у госпитализированных больных (Результаты Российского проспективного многоцентрового исследования). //Клиническая микробиология и антимикробная химиотерапия. – 2017. – Т. 19. – № 4. – С. 268–274.
- Сафин А. Л., Ачкасов С. И., Сухина М. А., Сушков О. И. Факторы риска развития диареи, ассоциированной с Clostridium diffi cile, у колопроктологических больных (обзор литературы) //Колопроктология. – 2017. – № 1. – С. 59–67.
- Kwon J. H., Olsen M. A., Dubberke E. R. Th e morbidity, mortality, and costs associated with Clostridium diffi cile infection //Infectious disease clinics of North America. – 2015. – Т. 29. – № 1. – С. 123–134.
- McGlone, S. M., Bailey, R. R., Zimmer, S. et al. Th e economic burden of Clostridium diffi cile //Clinical Microbiology and Infection. – 2012. – Т. 18. – № 3. – С. 282–289.
- Киргизов К. И., Шульга С. Ю., Пристанскова Е. А. и соавт. Энтероколит, связанный с Clostridium diffi cile, в детской гематологии-онкологии-решенная проблема? Обзор литературы и собственный опыт // Российский журнал детской гематологии и онкологии. – 2014. – № 1.
- O’Connor, J. R., Galang, M. A., Sambol, S. P. et al. Rifampin and rifaximin resistance in clinical isolates of Clostridium diffi cile //Antimicrobial agents and chemotherapy. – 2008. – Т. 52. – № 8. – С. 2813–2817.
- Bagdasarian N., Rao K., Malani P. N. Diagnosis and treatment of Clostridium diffi cile in adults: a systematic review //Jama. – 2015. – Т. 313. – № 4. – С. 398–408.
- Spigaglia, P., Barbanti, F., Mastrantonio, P. et al. Multidrug resistance in European Clostridium diffi cile clinical isolates //Journal of antimicrobial chemotherapy. – 2011. – Т. 66. – № 10. – С. 2227–2234.
- Lynch, T., Chong, P., Zhang, J. et al. Characterization of a stable, metronidazole-resistant Clostridium diffi cile clinical isolate //PLoS One. – 2013. – Т. 8. – № 1. – С. e53757.
- Dingle, K. E., Elliott, B., Robinson, E. et al. Evolutionary history of the Clostridium diffi cile pathogenicity locus // Genome biology and evolution. – 2013. – Т. 6. – № 1. – С. 36–52.
- Linkevicius M., Sandegren L., Andersson D. I. Potential of tetracycline resistance proteins to evolve tigecycline resistance //Antimicrobial agents and chemotherapy. – 2016. – Т. 60. – № 2. – С. 789–796.
- Spigaglia, P., Barbanti, F., Mastrantonio, P. et al. Fluoroquinolone resistance in Clostridium diffi cile isolates from Journal of medical microbiology. – 2008. – Т. 57. – № 6. – С. 784–789.
- Freeman, J., Baines, S. D., Jabes, D. et al. Comparison of the effi cacy of ramoplanin and vancomycin in both in vitro and in vivo models of clindamycin-induced Clostridium diffi cile infection //Journal of Antimicrobial Chemotherapy. – 2005. – Т. 56. – № 4. – С. 717–725.
- Shen J., Wang Y., Schwarz S. Presence and dissemination of the multiresistance gene cfr in Gram-positive and Gram-negative bacteria //Journal of Antimicrobial Chemotherapy. – 2013. – Т. 68. – № 8. – С. 1697–1706.
- Snydman, D. R., McDermott, L. A., Jacobus, N. V. et al. US-based national sentinel surveillance study for the epidemiology of Clostridium diffi cile-associated diarrheal isolates and their susceptibility to fi daxomicin // Antimicrobial agents and chemotherapy. – 2015. – Т. 59. – № 10. – С. 6437–6443.
- Peltier, J., Courtin, P., El Meouche, I. et al. Genomic and expression analysis of the vanG-like gene cluster of Clostridium diffi cile //Microbiology. – 2013. – Т. 159. – № 7. – С. 1510–1520.
- Spigaglia P. Recent advances in the understanding of antibiotic resistance in Clostridium diffi cile infection // Th erapeutic advances in infectious disease. – 2016. – Т. 3. – № 1. – С. 23–42.
- He, M., Miyajima, F., Roberts, P. et al. Emergence and global spread of epidemic healthcare-associated Clostridium diffi cile //Nature genetics. – 2013. – Т. 45. – № 1. – С. 109.
- Keessen, E. C., Hensgens, M. P., Spigaglia, P. et al. Antimicrobial susceptibility profi les of human and piglet Clostridium diffi cile PCR-ribotype 078 //Antimicrobial resistance and infection control. – 2013. – Т. 2. – № 1. – С. 14.
- Cohen, S. H., Gerding, D. N., Johnson, S. et al. Clinical practice guidelines for Clostridium diffi cile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA) //Infection Control & Hospital Epidemiology. – 2010. – Т. 31. – № 5. – С. 431–455.
- Goudarzi, M., Goudarzi, H., Alebouyeh, M. et al. Antimicrobial susceptibility of Clostridium diffi cile clinical isolates in Iran //Iranian Red Crescent Medical Journal. – 2013. – Т. 15. – № 8. – С. 704.
- Adler, A., Miller-Roll, T., Bradenstein, R et al. A national survey of the molecular epidemiology of Clostridium diffi cile in Israel: the dissemination of the ribotype 027 strain with reduced susceptibility to vancomycin and metronidazole //Diagnostic microbiology and infectious disease. – 2015. – Т. 83. – № 1. – С. 21–24.
- Freeman, J., Vernon, J., Morris, K. et al. Pan-European longitudinal surveillance of antibiotic resistance among prevalent Clostridium diffi cile ribotypes //Clinical Microbiology and Infection. – 2015. – Т. 21. – № 3. – С. 248. e9–248. e16.
- Jin, D., Luo, Y., Huang, C. et al. Molecular epidemiology of Clostridium diffi cile infection in hospitalized patients in Eastern China //Journal of clinical microbiology. – 2017. – Т. 55. – № 3. – С. 801–810.
- Ofosu A. Clostridium diffi cile infection: a review of current and emerging therapies //Annals of Gastroenterology: Quarterly Publication of the Hellenic Society of Gastroenterology. – 2016. – Т. 29. – № 2. – С. 147.
- Moura, I., Spigaglia, P., Barbanti, F., Mastrantonio, P. Analysis of metronidazole susceptibility in diff erent Clostridium diffi cile PCR ribotypes //Journal of Antimicrobial Chemotherapy. – 2012. – Т. 68. – № 2. – С. 362–365.
- Goudarzi, M., Goudarzi, H., Alebouyeh, M. et al. Antimicrobial susceptibility of Clostridium diffi cile clinical isolates in Iran //Iranian Red Crescent Medical Journal. – 2013. – Т. 15. – № 8. – С. 704.
- Peng, Z., Jin, D., Kim, H. B. et al. Update on antimicrobial resistance in Clostridium diffi cile: resistance mechanisms and antimicrobial susceptibility testing // Journal of clinical microbiology. – 2017. – Т. 55. – № 7. – С. 1998–2008.
- Cheng, J. W., Xiao, M., Kudinha, T., et al. Molecular epidemiology and antimicrobial susceptibility of Clostridium diffi cile isolates from a university teaching hospital in China //Frontiers in microbiology. – 2016. – Т. 7. – С. 1621.
- Leeds, J. A., Sachdeva, M., Mullin, S. et al. In vitro selection, via serial passage, of Clostridium diffi cile mutants with reduced susceptibility to fi daxomicin or vancomycin //Journal of Antimicrobial Chemotherapy. – 2013. – Т. 69. – № 1. – С. 41–44.
- Goldstein E. J. C., Babakhani F., Citron D. M. Antimicrobial activities of fi daxomicin //Clinical infectious diseases. – 2012. – Т. 55. – № suppl_2. – С. S143-S148.
- Kelly C. P., LaMont J. T. Clostridium diffi cile infection // Annual review of medicine. – 1998. – Т. 49. – № 1. – С. 375– 390.
- Cohen, S. H., Gerding, D. N., Johnson, S. et al. Clinical practice guidelines for Clostridium diffi cile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA) //Infection Control & Hospital Epidemiology. – 2010. – Т. 31. – № 5. – С. 431–455.
- Walkty, A., Boyd, D. A., Gravel, D. et al. Molecular characterization of moxifl oxacin resistance from Canadian Clostridium diffi cile clinical isolates //Diagnostic microbiology and infectious disease. – 2010. – Т. 66. – № 4. – С. 419–424.
- Wasels, F., Spigaglia, P., Barbanti, F., & Mastrantonio, P. Clostridium diffi cile erm (B)-containing elements and the burden on the in vitro fi tness //Journal of medical microbiology. – 2013. – Т. 62. – № 9. – С. 1461–1467.
- Rineh, A., Kelso, M. J., Vatansever, F. et al. Clostridium diffi cile infection: molecular pathogenesis and novel therapeutics //Expert review of anti-infective therapy. – 2014. – Т. 12. – № 1. – С. 131–150.
- Fry P. R., Th akur S., Gebreyes W. A. Antimicrobial resistance, toxinotype and genotypic profi ling of Clostridium diffi cile of swine origin //Journal of clinical microbiology. – 2012. – С. JCM. 06581–11.
- Kali A., Charles M. V. P., Srirangaraj S. Cadazolid: a new hope in the treatment of Clostridium diffi cile infection // Th e Australasian medical journal. – 2015. – Т. 8. – № 8. – С. 253.
- Norén, T., Alriksson, I., Åkerlund, T. et al. In vitro susceptibility to 17 antimicrobials of clinical Clostridium diffi cile isolates collected in 1993–2007 in Sweden // Clinical Microbiology and Infection. – 2010. – Т. 16. – № 8. – С. 1104–1110.
- Chong, P. M., Lynch, T., McCorrister, S. et al. Proteomic analysis of a NAP1 Clostridium diffi cile clinical isolate resistant to metronidazole //PloS one. – 2014. – Т. 9. – № 1. – С. e82622.
- Peng, Z., Addisu, A., Alrabaa, S., Sun, X. Antibiotic resistance and toxin production of Clostridium diffi cile isolates from the hospitalized patients in a large hospital in Florida //Frontiers in microbiology. – 2017. – Т. 8.
- Ðapa, T., Leuzzi, R., Ng, Y. K. et al. Multiple factors modulate biofi lm formation by the anaerobic pathogen Clostridium diffi cile //Journal of bacteriology. – 2013. – Т. 195. – № 3. – С. 545–555.
- Tyrrell, K. L., Citron, D. M., Warren, Y. A. et al. In vitro activities of daptomycin, vancomycin, and penicillin against Clostridium diffi cile, C. perfringens, Finegoldia magna, and Propionibacterium acnes //Antimicrobial agents and chemotherapy. – 2006. – Т. 50. – № 8. – С. 2728–2731
- Moura, I., Monot, M., Tani, C. et al. Multidisciplinary analysis of a nontoxigenic Clostridium diffi cile strain with stable resistance to metronidazole //Antimicrobial agents and chemotherapy. – 2014. – Т. 58. – № 8. – С. 4957–4960.
- Land K. M., Johnson P. J. Molecular basis of metronidazole resistance in pathogenic bacteria and protozoa //Drug Resistance Updates. – 1999. – Т. 2. – № 5. – С. 289–294.
- Baines S. D., Wilcox M. H. Antimicrobial resistance and reduced susceptibility in Clostridium diffi cile: potential consequences for induction, treatment, and recurrence of C. diffi cile infection //Antibiotics. – 2015. – Т. 4. – № 3. – С. 267–298.
- Peláez, T., Cercenado, E., Alcalá, L. et al. Metronidazole resistance in Clostridium diffi cile is heterogeneous // Journal of clinical microbiology. – 2008. – Т. 46. – № 9. – С. 3028–3032.
- Lebel S., Bouttier S., Lambert T. Th e cme gene of Clostridium diffi cile confers multidrug resistance in Enterococcus faecalis //FEMS microbiology letters. – 2004. – Т. 238. – № 1. – С. 93–100.
- Chopra I., Roberts M. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance //Microbiology and molecular biology reviews. – 2001. – Т. 65. – № 2. – С. 232–260.
- Saxton, K., Baines, S. D., Freeman, J. et al. Eff ects of exposure of Clostridium diffi cile PCR ribotypes 027 and 001 to fl uoroquinolones in a human gut model // Antimicrobial agents and chemotherapy. – 2009. – Т. 53. – № 2. – С. 412–420.
- Jasni, A. S., Mullany, P., Hussain, H., Roberts, A. P. Demonstration of conjugative transposon (Tn5397)-mediated horizontal gene transfer between Clostridium diffi cile and Enterococcus faecalis //Antimicrobial agents and chemotherapy. – 2010. – Т. 54. – № 11. – С. 4924–4926.
- Knetsch, C. W., Connor, T. R., Mutreja, A. et al. Whole genome sequencing reveals potential spread of Clostridium diffi cile between humans and farm animals in the Netherlands, 2002 to 2011 //Euro surveillance: bulletin Europeen sur les maladies transmissibles= European communicable disease bulletin. – 2014. – Т. 19. – № 45. – С. 20954.
- Kuwata, Y., Tanimoto, S., Sawabe, E. et al. Molecular epidemiology and antimicrobial susceptibility of Clostridium diffi cile isolated from a university teaching hospital in Japan //European Journal of Clinical Microbiology & Infectious Diseases. – 2015. – Т. 34. – № 4. – С. 763–772.
- Mullane K. Fidaxomicin in Clostridium diffi cile infection: latest evidence and clinical guidance //Th erapeutic advances in chronic disease. – 2014. – Т. 5. – № 2. – С. 69–84.
- Hächler H., Berger-Bächi B., Kayser F. H. Genetic characterization of a Clostridium diffi cile erythromycin-clindamycin resistance determinant that is transferable to Staphylococcus aureus //Antimicrobial agents and chemotherapy. – 1987. – Т. 31. – № 7. – С. 1039–1045.
- Norman, K. N., Scott, H. M., Harvey, R. B. et al. Comparison of antimicrobial susceptibility among Clostridium diffi cile isolated from an integrated human and swine population in Texas //Foodborne pathogens and disease. – 2014. – Т. 11. – № 4. – С. 257–264.
- Norén, T., Åkerlund, T., Wullt, M. et al. Mutations in fusA associated with posttherapy fusidic acid resistance in Clostridium diffi cile //Antimicrobial agents and chemotherapy. – 2007. – Т. 51. – № 5. – С. 1840–1843.
- Campbell, E. A., Korzheva, N., Mustaev, A., et al. Structural mechanism for rifampicin inhibition of bacterial RNA polymerase //Cell. – 2001. – Т. 104. – № 6. – С. 901–912.
- Aksoy D. Y., Unal S. New antimicrobial agents for the treatment of Gram‐positive bacterial infections //Clinical Microbiology and Infection. – 2008. – Т. 14. – № 5. – С. 411–420.
- Baines, S. D., Noel, A. R., Huscroft , G. S. et al. Evaluation of linezolid for the treatment of Clostridium diffi cile infection caused by epidemic strains using an in vitro human gut model //Journal of antimicrobial chemotherapy. – 2011. – Т. 66. – № 7. – С. 1537–1546.
- Ackermann, G., Tang, Y. J., Rodloff , A. C., et al. In vitro activity of sitafl oxacin against Clostridium diffi cile // Journal of Antimicrobial Chemotherapy. – 2001. – Т. 47. – № 5. – С. 722–724.
- Tenover F. C., Tickler I. A., Persing D. H. Antimicrobial-resistant strains of Clostridium diffi cile from North America //Antimicrobial agents and chemotherapy. – 2012. – Т. 56. – № 6. – С. 2929–2932.
- Marín, M., Martín, A., Alcalá, L. et al. Clostridium diffi cile isolates with high linezolid MICs harbor the multiresistance gene cfr //Antimicrobial agents and chemotherapy. – 2015. – Т. 59. – № 1. – С. 586–589.
- He, M., Miyajima, F., Roberts, P. et al. Emergence and global spread of epidemic healthcare-associated Clostridium diffi cile //Nature genetics. – 2013. – Т. 45. – № 1. – С. 109.
- Drudy, D., Quinn, T., O’mahony, R et al. High-level resistance to moxifl oxacin and gatifl oxacin associated with a novel mutation in gyrB in toxin-A-negative, toxin-B-positive Clostridium diffi cile //Journal of Antimicrobial Chemotherapy. – 2006. – Т. 58. – № 6. – С. 1264–1267.
- Dridi, L., Tankovic, J., Burghoff er, B. et al. gyrA and gyrB mutations are implicated in cross-resistance to ciprofl oxacin and moxifl oxacin in Clostridium diffi cile // Antimicrobial agents and chemotherapy. – 2002. – Т. 46. – № 11. – С. 3418–3421.
- Ackermann, G., Tang, Y. J., Kueper, R., et al. Resistance to Moxifl oxacin in ToxigenicClostridium diffi cile Isolates Is Associated with Mutations in gyrA //Antimicrobial agents and chemotherapy. – 2001. – Т. 45. – № 8. – С. 2348–2353.
- Putsathit, P., Maneerattanaporn, M., Piewngam, P. et al. Antimicrobial susceptibility of Clostridium diffi cile isolated in Th ailand //Antimicrobial Resistance & Infection Control. – 2017. – Т. 6. – № 1. – С. 58.
- Linder, J. A., Huang, E. S., Steinman, M. A. et al. Fluoroquinolone prescribing in the United States: 1995 to 2002 // Th e American journal of medicine. – 2005. – Т. 118. – № 3. – С. 259–268.
- Vincent, Y., Manji, A., Gregory-Miller, K., Lee, C. A review of management of Clostridium diffi cile infection: Primary and recurrence //Antibiotics. – 2015. – Т. 4. – № 4. – С. 411–423.
- Smith C. J., Markowitz S. M., Macrina F. L. Transferable tetracycline resistance in Clostridium diffi cile //Antimicrobial agents and chemotherapy. – 1981. – Т. 19. – № 6. – С. 997–1003.
- Drudy, D., Kyne, L., O’Mahony, R. et al. gyrA mutations in fl uoroquinolone-resistant Clostridium diffi cile PCR-027 // Emerging infectious diseases. – 2007. – Т. 13. – № 3. – С. 504.
- Mena, A., Riera, E., López-Causapé, C. et al. In vivo selection of moxifl oxacin-resistant Clostridium diffi cile // Antimicrobial agents and chemotherapy. – 2012. – Т. 56. – № 5. – С. 2788–2789.
- Lee, J. H., Lee, Y., Lee, K. et al. Th e changes of PCR ribotype and antimicrobial resistance of Clostridium diffi cile in a tertiary care hospital over 10 years //Journal of medical microbiology. – 2014. – Т. 63. – № 6. – С. 819–823.
- Chaparro-Rojas F., Mullane K. M. Emerging therapies for Clostridium diffi cile infection–focus on fi daxomicin // Infection and drug resistance. – 2013. – Т. 6. – С. 41.
- Johnson A. P., Wilcox M. H. Fidaxomicin: a new option for the treatment of Clostridium diffi cile infection // Journal of antimicrobial chemotherapy. – 2012. – Т. 67. – № 12. – С. 2788–2792.
- Erikstrup, L. T., Danielsen, T. K. L., Hall, V. et al. Antimicrobial susceptibility testing of Clostridium diffi cile using EUCAST epidemiological cut‐off values and disk diff usion correlates //Clinical Microbiology and Infection. – 2012. – Т. 18. – № 8.
- Pirš, T., Avberšek, J., Zdovc, I et al. Antimicrobial susceptibility of animal and human isolates of Clostridium diffi cile by broth microdilution //Journal of medical microbiology. – 2013. – Т. 62. – № 9. – С. 1478–1485.
- Wasels, F., Spigaglia, P., Barbanti, F. et al. Integration of erm (B)-containing elements through large chromosome fragment exchange in Clostridium diffi cile //Mobile genetic elements. – 2015. – Т. 5. – № 1. – С. 12–16.
- Fraga E. G., Nicodemo A. C., Sampaio J. L. M. Antimicrobial susceptibility of Brazilian Clostridium diffi cile strains determined by agar dilution and disk diff usion // Brazilian Journal of Infectious Diseases. – 2016. – Т. 20. – № 5. – С. 476–481.
- Mullany, P., Wilks, M., Lamb, I. et al. Genetic analysis of a tetracycline resistance element from Clostridium diffi cile and its conjugal transfer to and from Bacillus subtilis // Microbiology. – 1990. – Т. 136. – № 7. – С. 1343–1349.
Для цитирования:
Сухина М. А., Макешова А. Б., Шелыгин Ю. А., Кашников В. Н. Механизмы антибактериальной резистентности Clostridium (clostridioides) diffi cile. Экспериментальная и клиническая гастроэнтерология. 2018;160(12): 70–79. DOI: 10.31146/1682-8658-ecg-160-12-70-79
Загрузить полный текст
ОГЛАВЛЕНИЯ ВЫПУСКОВ
Контакты
Submission of the manuscript is online via e-mail
ecgarticle@gmail.com or
cholerez@mail.ru
Editorial Correspondence e-mail
gastrossr@gmail.com
Publishing, Subscriptions, Sales and Advertising, Correspondence e-mail
journal@cniig.ru
Tel: +7 917 561 9505
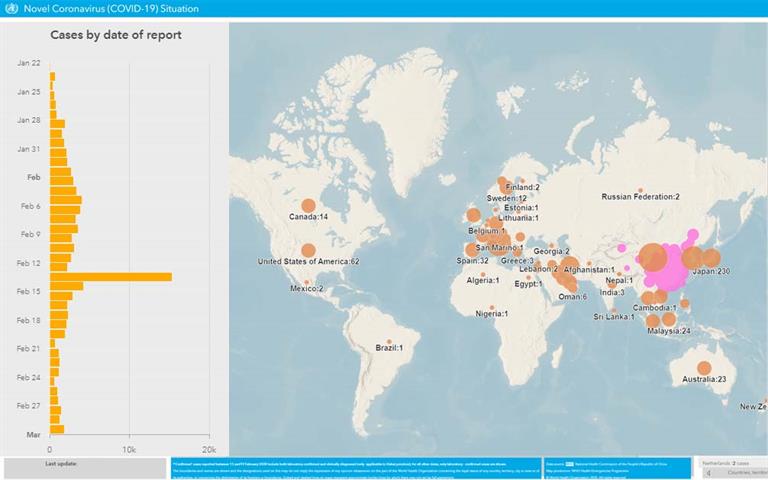
COVID-19