-
- ФГБОУ ВО РНИМУ им. Н. И. Пирогова (Москва, Россия)
- ФГАОУ ВО Первый МГМУ им. И. М. Сеченова (Москва, Россия)
- ГБУЗ «Ярославская областная клиническая онкологическая больница» (Ярославль, Москва)
- ФГБОУ ВО ЯГМУ Минздрава России (Ярославль, Москва)
- Национальный медицинский исследовательский центр здоровья детей (Москва, Россия)
Ключевые слова: эозинофильный эзофагит, эозинофилия пищевода, ингибиторы протонной помпы
Резюме: Цель. На примере собственных клинических наблюдений предствить обзор современой литературы, освещающей вопросы патогенеза, диагностики и лечения эозинофильного эзофагита (ЭоЭ). Основные положения. Эозинофильный эзофагит — это хроническое иммуноосредованное воспалительное заболевание пищевода. Диагностика ЭоЭ основана на характерной клинической картине дисфункции пищевода (дисфагия) в обязательной совокупности с выявлением эозинофильной инфильтрации слизистой оболочки пищевода при гистологическом исследовании. Базисная терапия эозинофильного эзофагита включает диетические ограничения, применение ингибиторов протонной помпы и топических кортикостероидов.
-
- Ивашкин В.Т., Баранская Е. К., Трухманов А. С., Кайбышева В. О. Эозинофильный эзофагит. М.: ООО «АИСПИ РАН»-М; 2013.
- Attwood SE, Smyrk TC and Demeester TRJJ. Esophageal eosinophilia with dysphagia. A distinct clinicopathologic syndrome. Dig. Dis. Sci. 1993; 38: 109–116.
- Straumann A, Spichtin HP, Bernoulli R, et al. Idiopathic eosinophilic esophagitis: a frequently overlooked disease with typical clinical aspects and discrete endoscopic fi ndings. Schweiz. Med. Wochenschr. 1994; 124: 1419–1429.
- Furuta GT, Liacouras CA, Collins MH, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology 2007; 133: 1342–1363.
- Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy. Clin.Immunol. 2011; 128: 3–20. https://doi.org/10.1016/j.jaci.2011.02.040
- Papadopoulou A, Koletzko S, Heuschkel R, et al. Management guidelines of eosinophilic esophagitis in childhood. J. Pediatr.Gastroenterol. Nutr. 2014; 58: 107–118. https:// doi.org/10.1097/MPG.0b013e3182a80be1
- Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol 2013; 108: 679–692. https://doi.org/10.1038/ajg.2013.71
- Ивашкин В.Т., Баранская Е. К., Кайбышева В. О., Трухманов А. С., Шептулин А. А. Клинические рекомендации по диагностике и лечению эозинофильного эзофагита. М., 2013.
- Lucendo AJ, Molina-Infante J, Arias Á, von Arnim U, Bredenoord AJ, Bussmann C, Amil Dias J, Bove M, González-Cervera J, Larsson H, Miehlke S, Papadopoulou A, Rodríguez-Sánchez J, Ravelli A, Ronkainen J, Santander C, Schoepfer AM, Storr MA, Terreehorst I, Straumann A, Attwood SE. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J. 2017; 5(3): 335–358. https://doi. org/10.1177/2050640616689525
- Arias A, Perez-Martinez I, Tenias JM, Lucendo AJ. Systematic review with meta- analysis: the incidence and prevalence of eosinophilic oesophagitis in children and adults in population-based studies. Aliment Pharmacol Th er 2016;43:3–15. https://doi.org/10.1111/apt.13441
- van Rhijn BD, Verheij J, Smout AJ, Bredenoord AJ. Rapidly increasing incidence of eosinophilic esophagitis in a large cohort. Neurogastroenterol Motil 2013;25:47–5. https://doi.org/10.1111/nmo.12009
- Warners M, de Rooij WE, Van Rhijn BD, Verheij J, Smout AJ, Bredenoord AJ. Large Increase in Incidence of Eosinophilc Esophagitis Over the Last 20 Years in the Netherlands: Results from a Nationwide Pathology Database. Gastroenterology 2017;152:862–863. https:// doi.org/10.1016/S0016–5085(17)32964–5
- Noel RJ, Putnam PE, Rothenberg ME. Eosinophilic esophagitis. N Engl J Med 2004;351:940–1.
- Dellon ES, Hirano I. Epidemiology and Natural History of Eosinophilic Esophagitis. Gastroenterology. 2018;154(2):319–332. https://doi.org/10.1053/j.gastro.2017.06.06
- Prasad GA, Alexander JA, Schleck CD, Zinsmeister AR, Smyrk TC, Elias RM, Locke GR, Talley NJ. Epidemiology of eosinophilic esophagitis over three decades in Olmsted County, Minnesota. Clin Gastroenterol Hepatol 2009;7:1055–61. https://doi.org/10.1016/j. cgh.2009.06.023
- Syed AA, Andrews CN, Shaff er E, Urbanski SJ, Beck P, Storr M. Th e rising incidence of eosinophilic oesophagitis is associated with increasing biopsy rates: a population-based study. Aliment Pharmacol Th er 2012;36:950– 8. https://doi.org/10.1111/apt.12053
- Dellon ES, Erichsen R, Baron JA, Shaheen NJ, Vyberg M, Sorensen HT, Pedersen L. Th e increasing incidence and prevalence of eosinophilic oesophagitis outpaces changes in endoscopic and biopsy practice: national population-based estimates from Denmark. Aliment Pharmacol Th er 2015;41:662–70. https://doi.org/10.1111/ apt.13129
- Giriens B, Yan P, Safroneeva E, Zwahlen M, Reinhard A, Nydegger A, Vavricka S, Sempoux C, Straumann A, Schoepfer AM. Escalating incidence of eosinophilic esophagitis in Canton of Vaud, Switzerland, 1993–2013: a population-based study. Allergy 2015;70:1633–9. https:// doi.org/10.1111/all.12733
- Straumann A, Simon HU. Eosinophilic esophagitis: escalating epidemiology? J Allergy Clin Immunol 2005;115:418–9. https://doi.org/10.1016/j.jaci.2004.11.006
- Straumann A, Simon HU. Eosinophilic esophagitis: escalating epidemiology? J Allergy Clin Immunol 2005;115:418–9. https://doi.org/10.1016/j.jaci.2004.11.006
- Arias A, Lucendo AJ. Prevalence of eosinophilic oesophagitis in adult patients in a central region of Spain. Eur J Gastroenterol Hepatol 2013;25:208–12. https://doi. org/10.1097/MEG.0b013e32835a4c95
- Homan M, Blagus R, Jeverica AK, Orel R. Pediatric Eosinophilic Esophagitis in Slovenia: Data From a Retrospective 2005–2012 Epidemiological Study. J Pediatr Gastroenterol Nutr 2015;61:313–8. https://doi.org/10.1097/ MPG.0000000000000797
- Dalby K, Nielsen RG, Kruse-Andersen S, Fenger C, Bindslev-Jensen C, Ljungberg S, Larsen K, Walsted AM, Husby S. Eosinophilic Oesophagitis in Infants and Children in the Region of Southern Denmark: A Prospective Study of Prevalence and Clinical Presentation. J Pediatr Gastroenterol Nutr 2010;51:280–2. https://doi.org/10.1097/ MPG.0b013e3181d1b107
- Spergel JM, Book WM, Mays E, Song L, Shah SS, Talley NJ, Bonis PA. Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States. J Pediatr Gastroenterol Nutr 2011;52:300–6. https://doi.org/10.1097/ MPG.0b013e3181eb5a9f
- Dellon ES, Jensen ET, Martin CF, Shaheen NJ, Kappelman MD. Prevalence of Eosinophilic Esophagitis in the United States. Clin Gastroenterol Hepatol 2014;12:589– 596. https://doi.org/10.1016/j.cgh.2013.09.008
- Maradey-Romero C, Prakash R, Lewis S, Perzynski A, Fass R. Th e 2011–2014 prevalence of eosinophilic oesophagitis in the elderly amongst 10 million patients in the United States. Aliment Pharmacol Th er 2015;41:1016–22. https://doi.org/10.1111/apt.13171
- Kim S, Sheikh J. Prevalence of eosinophilic esophagitis in a population-based cohort from Southern California. J Allergy Clin Immunol Pract 2015. https://doi. org/10.1016/j.jaip.2015.06.008
- Mansoor E, Cooper GS. Th e 2010–2015 Prevalence of Eosinophilic Esophagitis in the USA: A Population-Based Study. Dig Dis Sci 2016;61:2928–2934. https://doi. org/10.1007/s10620–016–4204–4
- Cherian S, Smith NM, Forbes DA. Rapidly increasing prevalence of eosinophilic oesophagitis in Western Australia. Arch Dis Child 2006;91:1000–1004.
- Sealock RJ, Rendon G, El-Serag HB. Systematic review: the epidemiology of eosinophilic oesophagitis in adults. Aliment Pharmacol Th er 2010;32:712–9.
- Molina-Infante J, Gonzalez-Cordero PL, Ferreira-Nossa HC, Mata-Romero P, Hernandez-Alonso M. Rising Incidence and Prevalence of Adult Eosinophilic Esophagitis in Caceres, Spain (2007–2016). Gastroenterology 2017;152:856. https://doi.org/10.1177/2050640617705913
- Fujiwara Y, Sugawa T, Tanaka F, Tatsuwaki H, Okuyama M, Hayakawa T, Yamamori K, Wada R, Ohtani K, Uno H, Tanigawa T, Watanabe Y, Tominaga K, Watanabe T, Takaishi O, Saeki Y, Nebiki H, Oshitani N, Sato H, Arakawa T. A multicenter study on the prevalence of Eosinophilic Esophagitis and PPI-responsive esophageal eosinophilic infi ltration. Intern Med 2012;51:3235–9.
- Fujishiro H, Amano Y, Kushiyama Y, Ishihara S, Kinoshita Y. Eosinophilic esophagitis investigated by upper gastrointestinal endoscopy in Japanese patients. J Gastroenterol 2011;46:1142–4. https://doi.org/10.1007/ s00535–011–0435–5
- Kinoshita Y, Furuta K, Ishimaura N, Ishihara S, Sato S, Maruyama R, Ohara S, Matsumoto T, Sakamoto C, Matsui T, Ishikawa S, Chiba T. Clinical characteristics of Japanese patients with eosinophilic esophagitis and eosinophilic gastroenteritis. J Gastroenterol 2013;48:333–9. https://doi.org/10.1007/s00535–012–0640-x
- Kinoshita Y, Ishimura N, Oshima N, Ishihara S. Systematic review: Eosinophilic esophagitis in Asian countries. World J Gastroenterol 2015;21:8433–40. https:// doi.org/10.3748/wjg.v21.i27.8433
- Shi YN, Sun SJ, Xiong LS, Cao QH, Cui Y, Chen MH. Prevalence, clinical manifestations and endoscopic features of eosinophilic esophagitis: a pathological review in China. J Dig Dis 2012;13:304–9. https://doi.org/10.1111/j.1751– 2980.2012.00593.x
- Joo MK, Park JJ, Kim SH, Kim KH, Jung W, Yun JW, Lee BJ, Kim JH, Yeon JE, Kim JS, Byun KS, Lee SW, Bak YT. Prevalence and endoscopic features of eosinophilic esophagitis in patients with esophageal or upper gastrointestinal symptoms. J Dig Dis 2012;13:296–303. https://doi. org/10.1111/j.1751–2980.2012.00589.x
- Altun R, Akbas E, Yildirim AE, Ocal S, Korkmaz M, Selcuk H. Frequency of eosinophilic esophagitis in patients with esophageal symptoms: a single-center Turkish experience. Dis Esophagus 2013;26:776–81. https://doi. org/10.1111/j.1442–2050.2012.01395.x
- Assiri AM, Saeed A. Incidence and diagnostic features of eosinophilic esophagitis in a group of children with dysphagia and gastroesophageal refl ux disease. Saudi Med J 2014;35:292–7.
- Foroutan M, Norouzi A, Molaei M, Mirbagheri SA, Irvani S, Sadeghi A, Derakhshan F, Tavassoli S, Besharat S, Zali M. Eosinophilic Esophagitis in Patients with Refractory Gastroesophageal Refl ux Disease. Dig Dis Sci 2010;55:28–31. https://doi.org/10.1007/s10620–008–0706-z
- Hasosah MY, Sukkar GA, Alsahafi AF, Thabit AO, Fakeeh ME, Al-Zahrani DM, Satti MB. Eosinophilic esophagitis in Saudi children: symptoms, histology and endoscopy results. Saudi J Gastroenterol 2011;17:119–23. https://doi.org/10.4103/1319–3767.77242
- Niranjan R, Th akur AK, Mishra A. Food allergy and eosinophilic esophagitis in India: Lack of diagnosis. Indian J Gastroenterol 2016;35:72–3. https://doi.org/10.1007/ s12664–016–0629–0
- Aceves SS, Newbury RO, Dohil R, Schwimmer J, Bastian JF. Distinguishing eosinophilic esophagitis in pediatric patients: clinical, endoscopic, and histologic features of an emerging disorder. J Clin Gastroenterol 2007;41:252–6.
- Veerappan GR, Perry JL, Duncan TJ, Baker TP, Maydonovitch C, Lake JM, Wong RK, Osgard EM. Prevalence of Eosinophilic Esophagitis in an Adult Population Undergoing Upper Endoscopy: A Prospective Study. Clin Gastroenterol Hepatol 2009;7:420–426.
- Desai TK, Stecevic V, Chang CH, Goldstein NS, Badizadegan K, Furuta GT. Association of eosinophilic infl ammation with esophageal food impaction in adults. Gastrointest Endosc 2005;61:795–801.
- Kerlin P, Jones D, Remedios M, Campbell C. Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus. J Clin Gastroenterol 2007;41:356–61.
- Byrne KR, Panagiotakis PH, Hilden K, Th omas KL, Peterson KA, Fang JC. Retrospective Analysis of Esophageal Food Impaction: Diff erences in Etiology by Age and Gender. Dig Dis Sci 2007.
- Kirchner GI, Zuber-Jerger I, Endlicher E, Gelbmann C, Ott C, Ruemmele P, Scholmerich J, Klebl F. Causes of bolus impaction in the esophagus. Surg Endosc 2011;25:3170–4. https://doi.org/10.1007/s00464–011–1681–6
- Sperry SL, Crockett SD, Miller CB, Shaheen NJ, Dellon ES. Esophageal foreign-body impactions: epidemiology, time trends, and the impact of the increasing prevalence of eosinophilic esophagitis. Gastrointest Endosc 2011;74:985–91. https://doi.org/10.1016/j.gie.2011.06.029
- Hurtado CW, Furuta GT, Kramer RE. Etiology of esophageal food impactions in children. J Pediatr Gastroenterol Nutr 2011;52:43–6. https://doi.org/10.1097/ MPG.0b013e3181e67072
- Diniz LO, Towbin AJ. Causes of Esophageal Food Bolus Impaction in the Pediatric Population. Dig Dis Sci 2011. https://doi.org/10.1007/s10620–011–1911–8
- Mahesh VN, Holloway RH, Nguyen NQ. Changing epidemiology of food bolus impaction: is eosinophilic esophagitis to blame? J Gastroenterol Hepatol 2013;28:963–6. https://doi.org/10.1111/jgh.12135
- Philpott H, Nandurkar S, Th ien F, Bloom S, Lin E, Goldberg R, Boyapati R, Finch A, Royce SG, Gibson PR. Seasonal Recurrence of Food Bolus Obstruction in Eosinophilic Esophagitis. Intern Med J 2015;45:939–43. https://doi. org/10.1111/imj.12790
- Hiremath GS, Hameed F, Pacheco A, Olive A, Davis CM, Shulman RJ. Esophageal Food Impaction and Eosinophilic Esophagitis: A Retrospective Study, Systematic Review, and Meta-Analysis. Dig Dis Sci 2015;60:3181–93. https://doi.org/10.1007/s10620–015–3723–8
- Gretarsdottir HM, Jonasson JG, Bjornsson ES. Etiology and management of esophageal food impaction: a population based study. Scand J Gastroenterol 2015;50:513–8. https://doi.org/10.3109/00365521.2014.983159
- Truskaite K, Dlugosz A. Prevalence of Eosinophilic Esophagitis and Lymphocytic Esophagitis in Adults with Esophageal Food Bolus Impaction. Gastroenterol Res Pract 2016; https://doi.org/10.1155/2016/9303858
- Dellon ES, Kim HP, Sperry SL, Rybnicek DA, Woosley JT, Shaheen NJ. A phenotypic analysis shows that eosinophilic esophagitis is a progressive fi brostenotic disease. Gastrointest Endosc 2014;79:577–85. https://doi. org/10.1016/j.gie.2013.10.027
- Schoepfer AM, Safroneeva E, Bussmann C, Kuchen T, Portmann S, Simon HU, Straumann A. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology 2013;145:1230–1236. https://doi.org/10.1053/j.gastro.2013.08.015
- Lipka S, Kumar A, Richter JE. Impact of Diagnostic Delay and Other Risk Factors on Eosinophilic Esophagitis Phenotype and Esophageal Diameter. J Clin Gastroenterol 2016;50:134–40. https://doi.org/10.1097/ MCG.0000000000000297
- Butz BK, Wen T, Gleich GJ, Furuta GT, Spergel J, King E, Kramer RE, Collins MH, Stucke E, Mangeot C, Jackson WD, O’Gorman M, Abonia JP, Pentiuk S, Putnam PE, Rothenberg ME. Effi cacy, Dose Reduction, and Resistance to High-dose Fluticasone in Patients with Eosinophilic Esophagitis. Gastroenterology 2014;147:324–33. https:// doi.org/10.1053/j.gastro.2014.04.019
- Miehlke S, Hruz P, Vieth M, Bussmann C, von Arnim U, Bajbouj M, Schlag C, Madisch A, Fibbe C, Wittenburg H, Allescher HD, Reinshagen M, Schubert S, Tack J, Muller M, Krummenerl P, Arts J, Mueller R, Dilger K, Greinwald R, Straumann A. A randomised, double-blind trial comparing budesonide formulations and dosages for short-term treatment of eosinophilic oesophagitis. Gut 2016;65:390– 9. https://doi.org/10.1136/gutjnl-2014–308815
- Schoepfer AM, Gonsalves N, Bussmann C, Conus S, Simon HU, Straumann A, Hirano I. Esophageal dilation in eosinophilic esophagitis: eff ectiveness, safety, and impact on the underlying infl ammation. Am J Gastroenterol 2010;105:1062–70. https://doi.org/ 10.1038/ajg.2009.657
- Koutlas NT, Dellon ES. Progression from an infl ammatory to a fi brostenotic phenotype in eosinophilic esophagitis. Case Rep Gastroenterol 2017. https://doi. org/10.1159/000477391
- O’Shea KM, Aceves SS, Dellon ES, Gupta SK, Spergel JM, Furuta GT, Rothenberg ME. Pathophysiology of Eosinophilic Esophagitis. Gastroenterology. 2018 Jan;154(2):333–345. https://doi.org/10.1053/j.gastro.2017.06.065
- Rochman M, Travers J, Miracle CE, et al. Profound loss of esophageal tissue diff erentiation in patients with eosinophilic esophagitis. J Allergy Clin Immunol; 2017: S0091–6749(17)30036–2. https://doi.org/10.1016/j. jaci.2016.11.042
- Litosh VA, Rochman M, Rymer JK, Porollo A, Kottyan LC, Rothenberg ME. Calpain-14 and its association with eosinophilic esophagitis. Th e Journal of Allergy and Clinical Immunology;2017: S0091–6749(16)31215–5. https://doi.org/101016/jjaci201609027
- Kottyan LC, Davis BP, Sherrill JD, et al. Genome-wide association analysis of eosinophilic esophagitis provides insight into the tissue specifi city of this allergic disease. Nat Genet 2014;46:895–900. https://doi.org/10.1038/ ng.303
- Blanchard C, Wang N, Stringer KF, et al. Eotaxin-3 and a uniquely conserved gene-expression profi le in eosinophilic esophagitis. J Clin Invest 2006;116:536–47.
- Blanchard C, Mingler MK, Vicario M, et al. IL-13 involvement in eosinophilic esophagitis: transcriptome analysis and reversibility with glucocorticoids. J Allergy Clin Immunol 2007;120:1292–300.
- Kitajima M, Lee HC, Nakayama T, Ziegler SF. TSLP enhances the function of helper type 2 cells. Eur J Immunol 2011;41:1862–71. https://doi.org/10.1002/eji.201041195
- Hui CC, Rusta-Sallehy S, Asher I, Heroux D, Denburg JA. Th e eff ects of thymic stromal lymphopoietin and IL-3 on human eosinophil-basophil lineage commitment: Relevance to atopic sensitization. Immun Infl amm Dis 2014;2:44–55. https://dx.doi.org/10.1002%2Fiid3.20
- Wen T, Stucke EM, Grotjan TM, Kemme KA, Abonia JP, et al. Molecular diagnosis of eosinophilic esophagitis by gene expression profiling. Gastroenterology. 2013; 145(6):1289–99. https://doi.org/10.1053/j.gastro.2013.08.046
- Davis BP, Rothenberg ME. Mechanisms of Disease of Eosinophilic Esophagitis. Annual review of pathology. 2016;11:365–393. https://doi.org/10.1146/annurev-pathol-012615–044241
- Lipka S, Kumar A, Richter JE. Impact of Diagnostic Delay and Other Risk Factors on Eosinophilic Esophagitis Phenotype and Esophageal Diameter. J Clin Gastroenterol 2016;50:134–40. https://doi.org/10.1097/ MCG.0000000000000297
- Abdulnour-Nakhoul SM, Al-Tawil Y, Gyft opoulos AA, Brown KL, Hansen M, et al. Alterations in junctional proteins, infl ammatory mediators and extracellular matrix molecules in eosinophilic esophagitis. Clin Immunol. 2013; 148(2):265–78. https://doi.org/10.1016/j. clim.2013.05.004
- Blanchard C, Stucke EM, Burwinkel K, Caldwell JM, Collins MH, et al. Coordinate interaction between IL-13 and epithelial diff erentiation cluster genes in eosinophilic esophagitis. J Immunol. 2010; 184(7):4033–41. https:// doi.org/10.4049/jimmunol.0903069
- Davis BP, Kottyan LC, Stucke EM, Sherrill JD, Rothenberg ME. Functional analysis of calpain-14 in eosinophilic esophagitis. J Allergy Clin Immunol. 2015; 135(2): AB247. https://doi.org/10.1016/j.jaci.2014.12.1184
- Samuelov L, Sarig O, Harmon RM, et al. Desmoglein 1 defi ciency results in severe dermatitis, multiple allergies and metabolic wasting. Nat Genet 2013;45:1244–8. https://doi.org/10.1038/ng.2739
- Steinbach EC, Hernandez M, Dellon ES. Eosinophilic Esophagitis and the Eosinophilic Gastrointestinal Diseases: Approach to Diagnosis and Management. J Allergy Clin Immunol Pract. 2018 Sep – Oct;6(5):1483–1495. https://doi.org/10.1016/j.jaip.2018.06.012201.
- Hirano I. How to Approach a Patient With Eosinophilic Esophagitis. Gastroenterology. 2018 Sep;155(3):601–606. https://doi.org/j.gastro.2018.08.001.
- Dellon ES, Liacouras CA, Molina-Infante J et al. Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. Gastroenterology. 2018 Sep 6. pii: S0016–5085(18)34763–2. https://doi.org/10.1053/j.gastro.2018.07.009.
- Straumann A, Katzka DA. Diagnosis and Treatment of Eosinophilic Esophagitis. Gastroenterology. 2018 Jan;154(2):346–359. https://doi.org/10.1053/j.gastro.2017.05.066
- Dellon ES. Diagnosis and management of eosinophilic esophagitis. Clin Gastroenterol Hepatol 2012;10:1066–78 https://doi.org/10.1016/j.cgh.2012.06.00
- Lucendo AJ, Friginal-Ruiz AB, Rodriguez B. Boerhaave’s syndrome as the primary manifestation of adult eosinophilic esophagitis. Two case reports and a review of the literature. Dis Esophagus 2011;24: E11–5. https://doi. org/10.1111/j.1442–2050.2010.01167.x
- Straumann A, Bussmann C, Zuber M, et al. Eosinophilic esophagitis: analysis of food impaction and perforation in 251 adolescent and adult patients. Clin Gastroenterol Hepatol 2008;6:598–600. https://doi.org/10.1016/j. cgh.2008.02.003
- Jackson WE, Mehendiratta V, Palazzo J, et al. Boerhaave’s syndrome as an initial presentation of eosinophilic esophagitis: a case series. Ann Gastroenterol 2013;26:166–169.
- Hirano I, Moy N, Heckman MG, et al. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: validation of a novel classifi cation and grading system. Gut 2013;62:489–95. https://doi.org/10.1136/ gutjnl-2011–301817
- Kim HP, Vance RB, Shaheen NJ, et al. Th e prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:988–96 https://doi.org/10.1016/j.cgh.2012.04.019
- Dellon ES, Cotton CC, Gebhart JH, et al. Accuracy of the eosinophilic esophagitis endoscopic reference score in diagnosis and determining response to treatment. Clin Gastroenterol Hepatol 2016;14:31–39. 1 https://doi. org/0.1016/j.cgh.2015.08.040
- van Rhijn BD, Warners MJ, Curvers WL, et al. Evaluating the endoscopic reference score for eosinophilic esophagitis: moderate to substantial intra- and interobserver reliability. Endoscopy 2014;46:1049–1055. https://doi. org/10.1055/s-0034–1377781
- Rodriguez-Sanchez J, Barrio-Andres J, Nantes Castillejo O, et al. Th e Endoscopic Reference Score shows modest accuracy to predict either clinical or histological activity in adult patients with eosinophilic oesophagitis. Aliment Pharmacol Th er 2017;45:300–309. https://doi. org/10.1111/apt.13845
- Dellon ES, Gibbs WB, Fritchie KJ, et al. Clinical, endoscopic, and histologic fi ndings distinguish eosinophilic esophagitis from gastroesophageal refl ux disease. Clin Gastroenterol Hepatol 2009;7:1305–13; https://doi. org/10.1016/j.cgh.2009.08.030
- Moawad FJ, Robinson CL, Veerappan GR, et al. Th e tug sign: an endoscopic feature of eosinophilic esophagitis. Am J Gastroenterol 2013;108:1938–9. https://doi. org/10.1038/ajg.2013.252
- Gonsalves N, Policarpio-Nicolas M, Zhang Q, et al. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointest Endosc 2006;64:313–9. https://doi.org/10.1016/j. gie.2006.04.037
- Collins MH, Martin LJ, Alexander ES, et al. Newly developed and validated eosinophilic esophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosis and monitoring. Dis Esophagus 2016. https://doi.org/10.1111/dote.12470
- Menard-Katcher C, Swerdlow MP, Mehta P, et al. Contribution of Esophagram to the Evaluation of Complicated Pediatric Eosinophilic Esophagitis. J Pediatr Gastroenterol Nutr 2015;61:541–6. https://doi.org/10.1097/ MPG.0000000000000849
- Podboy A, Katzka DA, Enders F, et al. Oesophageal narrowing on barium oesophagram is more common in adult patients with eosinophilic oesophagitis than PPI-responsive oesophageal eosinophilia. Aliment Pharmacol Th er 2016;43:1168–77. https://doi.org/10.1111/ apt.13601
- Konikoff MR, Blanchard C, Kirby C, et al. Potential of blood eosinophils, eosinophil-derived neurotoxin, and eotaxin-3 as biomarkers of eosinophilic esophagitis. Clin Gastroenterol Hepatol 2006;4:1328–1336.
- Rodriguez-Sanchez J, Gomez-Torrijos E, de-la-SantaBelda E, et al. Eff ectiveness of serological markers of eosinophil activity in monitoring eosinophilic esophagitis. Rev Esp Enferm Dig 2013;105:462–467.
- Schlag C, Miehlke S, Heiseke A, et al. Peripheral blood eosinophils and other non-invasive biomarkers can monitor treatment response in eosinophilic oesophagitis. Aliment Pharmacol Th er 2015;42:1122–1130. https://doi. org/10.1111/apt.13386
- Min SB, Nylund CM, Baker TP, Ally M, Reinhardt B, Chen YJ, Nazareno L, Moawad FJ. Longitudinal Evaluation of Noninvasive Biomarkers for Eosinophilic Esophagitis. J Clin Gastroenterol. 2017;51(2):127–135. https://doi. org/10.1097/MCG.0000000000000621
- Dellon ES, Rusin S, Gebhart JH, et al. Utility of a noninvasive serum biomarker panel for diagnosis and monitoring of eosinophilic esophagitis: a prospective study. Am J Gastroenterol 2015;110:821–827. https://doi. org/10.1038/ajg.2015.57
- Schaefer ET, Fitzgerald JF, Molleston JP, et al. Comparison of oral prednisone and topical fl uticasone in the treatment of eosinophilic esophagitis: a randomized trial in children. Clin Gastroenterol Hepatol 2008;6:165 https://doi.org/10.1016/j.cgh.2007.11.008
- Alexander JA, Jung KW, Arora AS, et al. Swallowed fl uticasone improves histologic but not symptomatic response of adults with eosinophilic esophagitis. Clin Gastroenterol Hepatol 2012;10:742–749. https://doi. org/10.1016/j.cgh.2012.03.018
- Gupta SK, Vitanza JM, Collins MH. Effi cacy and safety of oral budesonide suspension in pediatric patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol 2015;13:66–76. https://doi.org/10.1016/j.cgh.2014.05.021
- Dohil R, Newbury R, Fox L, et al. Oral viscous budesonide is eff ective in children with eosinophilic esophagitis in a randomized, placebo-controlled trial. Gastroenterology 2010;139:418–429. https://doi.org/10.1053/j. gastro.2010.05.001
- Konikoff MR, Noel RJ, Blanchard C, et al. A randomized, double-blind, placebo- controlled trial of fl uticasone propionate for pediatric eosinophilic esophagitis. Gastroenterology 2006;131:1381–1391.
- Dellon ES, Sheikh A, Speck O, et al. Viscous topical is more eff ective than nebulized steroid therapy for patients with eosinophilic esophagitis. Gastroenterology 2012;143:321–324. https://doi.org/10.1053/j.gastro.2012.04.049
- Butz BK, Wen T, Gleich GJ, et al. Efficacy, dose reduction, and resistance to high-dose fluticasone in patients with eosinophilic esophagitis. Gastroenterology 2014;147:324–333. https://doi.org/10.1053/j.gastro.2014.04.019
- Miehlke S, Hruz P, Vieth M, et al. A randomised, double-blind trial comparing budesonide formulations and dosages for short-term treatment of eosinophilic oesophagitis. Gut 2016;65:390–399. https://doi.org/10.1136/ gutjnl-2014–308815
- Tan N Di, Xiao YL, Chen MH. Steroids therapy for eosinophilic esophagitis: Systematic review and meta-analysis. J Dig Dis 2015;16:431–442. https://doi.org/10.1111/1751– 2980.12265
- Sawas T, Dhalla S, Sayyar M, et al. Systematic review with meta-analysis: pharmacological interventions for eosinophilic oesophagitis. Aliment Pharmacol Th er 2015;41:797–806. https://doi.org/10.1111/apt.13147
- Murali AR, Gupta A, Attar BM, et al. Topical steroids in eosinophilic esophagitis: systematic review and meta-analysis of placebo controlled randomized clinical trials. J Gastroenterol Hepatol 2015; 31:1111–1119. https:// doi.org/10.1111/jgh.13281
- Chuang M-YA, Chinnaratha MA, Hancock DG, et al. Topical steroid therapy for the treatment of eosinophilic esophagitis (EoE): a systematic review and meta- analysis. Clin Transl Gastroenterol 2015;6: e82. https://doi. org/10.1038/ctg.2015.9
- Moawad FJ, Veerappan GR, Dias JA, et al. Randomized controlled trial comparing aerosolized swallowed fl uticasone to esomeprazole for esophageal eosinophilia. Am J Gastroenterol 2013;108:366–372. https://doi. org/10.1038/ajg.2012.443
- Peterson KA, Th omas KL, Hilden K, et al. Comparison of esomeprazole to aerosolized, swallowed fl uticasone for eosinophilic esophagitis. Dig Dis Sci 2010;55:1313–1319. https://doi.org/10.1007/s10620–009–0859–4
- Straumann A, Conus S, Degen L, Frei C, Bussmann C, Beglinger C, Schoepfer A, Simon HU. Long-term budesonide maintenance treatment is partially eff ective for patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol 2011;9:400–9. https://doi.org/10.1016/j. cgh.2011.01.017
- Cheng E, Zhang X, Huo X, Yu C, Zhang Q, Wang DH, Spechler SJ, Souza RF. Omeprazole blocks eotaxin-3 expression by oesophageal squamous cells from patients with eosinophilic oesophagitis and GORD. Gut. 2013 Jun;62(6):824–32. https://doi.org/10.1136/gutjnl-2012–302250.
- Ngo P, Furuta GT, Antonioli DA, et al. Eosinophils in the esophagus – peptic or allergic eosinophilic esophagitis? Case series of three patients with esophageal eosinophilia. Am J Gastroenterol 2006;101:1666–1670.
- Dranove JE, Horn DS, Davis MA, et al. Predictors of response to proton pump inhibitor therapy among children with signifi cant esophageal eosinophilia. J Pediatr 2009;154:96–100. https://doi.org/10.1016/j. jpeds.2008.07.042
- Molina-Infante J, Ferrando-Lamana L, Ripoll C, et al. Esophageal eosinophilic infi ltration responds to proton pump inhibition in most adults. Clin Gastroenterol Hepatol 2011; 9: 110–117. https://doi.org/10.1016/j. cgh.2010.09.019
- Gutierrez-Junquera C, Fernandez-Fernandez S, Cilleruelo ML, et al. High revalence of response to proton-pump inhibitor treatment in children with esophageal eosinophilia. J Pediatr Gastroenterol Nutr 2016;62:704–710. https://doi.org/10.1097/MPG.0000000000001019
- Lucendo AJ, Arias A, Molina-Infante J. Effi cacy of proton pump inhibitor drugs for inducing clinical and histologic remission in patients with symptomatic esophageal eosinophilia: a systematic review an d meta-analysis. Clin Gastroenterol Hepatol 2016;14:13–22. https://doi. org/10.1016/j.cgh.2015.07.041
- Cheng E, Zhang X, Wilson KS, Wang DH, Park JY, Huo X, Yu C, Zhang Q, Spechler SJ, Souza RF. JAK-STAT6 Pathway Inhibitors Block Eotaxin-3 Secretion by Epithelial Cells and Fibroblasts from Esophageal Eosinophilia Patients: Promising Agents to Improve Infl ammation and Prevent Fibrosis in Eo E. PLoS One. 2016 Jun 16;11(6): e0157376. https://doi.org/10.1371/journal.pone.0157376.
- Dellon ES, Liacouras CA. Advances in clinical management of eosinophilic esophagitis. Gastroenterology 2014;147:1238–1254. https://doi.org/10.1053/j.gastro.2014.07.055
- Attwood SEA, Lewis CJ, Bronder CS, et al. Eosinophilic oesophagitis: a novel treatment using Montelukast. Gut 2003;52:181–185.
- Stumphy J, Al-Zubeidi D, Guerin L, Mitros F, Rahhal R. Observations on use of montelukast in pediatric eosinophilic esophagitis: insights for the future. Dis Esophagus. Australia; 2011;24(4):229–34. https://doi. org/10.1111/j.1442–2050.2010.01134.x
- Alexander JA, Ravi K, Enders FT, Geno DM, Kryzer LA, Mara KC, Smyrk TC, Katzka DA. Montelukast Does not Maintain Symptom Remission Aft er Topical Steroid Th erapy for Eosinophilic Esophagitis. Clin Gastroenterol Hepatol. 2017;15(2):214–221.e2. https://doi.org/10.1016/j. cgh.2016.09.013
- . Lucendo AJ, De Rezende LC, Jimenez-Contreras S, et al. Montelukast was ineffi cient in maintaining steroid-induced remission in adult eosinophilic esophagitis. Dig Dis Sci 2011;56:3551–3558. https://doi.org/10.1007/ s10620–011–1775-y
- Rothenberg ME, Wen T, Greenberg A, et al. Intravenous anti-IL-13 mAb QAX576 for the treatment of eosinophilic esophagitis. J Allergy Clin Immunol 2015;135:500–7. https://doi.org/10.1016/j.jaci.2014.07.049.
- Dellon ES, Collins M, Assouline-Dayan Y, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of a Novel Recombinant, Humanized, Anti-Interleukin-13 Monoclonal Antibody (RPC4046) in Patients with Active Eosinophilic Esophagitis: Results of the HEROES Study. American Journal of Gastroenterology 2016;111: S186-S186.
- Straumann A, Bussmann C, Conus S, et al. Anti-TNF-alpha (infl iximab) therapy for severe adult eosinophilic esophagitis. J Allergy Clin Immunol 2008;122:425–7. https://doi.org/10.1016/j.jaci.2008.06.012
- Kelly KJ, Lazenby AJ, Rowe PC, et al. Eosinophilic esophagitis attributed to gastroesophageal refl ux: improvement with an amino acid-based formula. Gastroenterology 1995;109:1503–1512.
- Arias A, Gonzalez-Cervera J, Tenias JM, et al. Effi cacy of dietary interventions for inducing histologic remission in patients with eosinophilic esophagitis: a systematic review and meta-analysis. Gastroenterology 2014;146:1639–1648. https://doi.org/10.1053/j.gastro.2014.02.006
- Peterson KA, Byrne KR, Vinson LA, et al. Elemental diet induces histologic response in adult eosinophilic esophagitis. Am J Gastroenterol 2013;108:759–766. https://doi. org/10.1038/ajg.2012.468
- Liacouras CA, Spergel JM, Ruchelli E, et al. Eosinophilic esophagitis: A 10-year experience in 381 children. Clin Gastroenterol Hepatol 2005;3:1198–1206
- Spergel JM, Beausoleil JL, Mascarenhas M, et al. Th e use of skin prick tests and patch tests to identify causative foods in eosinophilic esophagitis. J Allergy Clin Immunol 2002;109:363–368.
- Spergel JM, Brown-Whitehorn TF, Cianferoni A, et al. Identifi cation of causative foods in children with eosinophilic esophagitis treated with an elimination diet. J Allergy Clin Immunol 2012;130:461–467. https://doi. org/10.1016/j.jaci.2012.05.021
- Kagalwalla AF, Shah A, Ritz S, et al. Cow’s milk protein-induced eosinophilic esophagitis in a child with gluten-sensitive enteropathy. J Pediatr Gastroenterol Nutr 2007;44:386–388. https://doi.org/10.1097/01. mpg.0000243430.32087.5c
- Wolf WA, Jerath MR, Sperry SLW, et al. Dietary elimination therapy is an eff ective option for adults with eosinophilic esophagitis. Clin Gastroenterol Hepatol 2014;12:1272–1279. https://doi.org/10.1016/j. cgh.2013.12.034
- Molina-Infante J, Martin-Noguerol E, Alvarado-A renas M, et al. Selective elimination diet based on skin testing has suboptimal effi cacy for adult eosinophilic esophagitis. J Allergy Clin Immunol 2012;130:1200–1202. https:// doi.org/10.1016/j.jaci.2012.06.027
- Philpott H, Nandurkar S, Royce SG, et al. Allergy tests do not predict food triggers in adult patients with eosinophilic oesophagitis. A comprehensive prospective study using fi ve modalities. Aliment Pharmacol Th er 2016;44:223–233. https://doi.org/10.1111/apt.13676
- Kagalwalla AF, Sentongo TA, Ritz S, et al. Eff ect of sixfood elimination diet on clinical and histologic outcomes in eosinophilic esophagitis. Clin Gastroenterol Hepatol 2006;4:1097–1102.
- Kagalwalla AF, Shah A, Li BUK, et al. Identifi cation of specifi c foods responsible for infl ammation in children with eosinophilic esophagitis successfully treated with empiric elimination diet. J Pediatr Gastroenterol Nutr 2011;53:145–149. https://doi.org/10.1097/MPG. 0b013e31821cf503
- Molina-Infante J, Arias A, Barrio J, et al. Four-food group elimination diet for adult eosinophilic esophagitis: A prospective multicenter study. J Allergy Clin Immunol 2014;134:1093–1099. https://doi.org/10.1016/j. jaci.2014.07.023
- Kagalwalla A, Amsden K, Makhija MM, et al. A multicenter study assessing the clinical, endoscopic and histologic response to four food elimination diet for the treatment of eosinophilic esophagitis. Gastroenterology 2015;148:30. https://doi.org/10.1016/S0016– 5085(15)30103–7
- Kagalwalla AF, Amsden K, Shah A, et al. Cow’s milk elimination: a novel dietary approach to treat eosinophilic esophagitis. J Pediatr Gastroenterol Nutr 2012;55:711–716. https://doi.org/10.1097/MPG.0b013e318268da40
- Kruszewski PG, Russo JM, Franciosi JP, et al. Prospective, comparative eff ectiveness trial of cow’s milk elimination and swallowed fl uticasone for pediatric eosinophilic esophagitis. Dis Esophagus 2016;29:377–384. https:// doi.org/10.1111/dote.12339
- Molina-Infante J, Arias Á, Alcedo J, Garcia-Romero R, Casabona-Frances S, Prieto-Garcia A, Modolell I, Gonzalez-Cordero PL, Perez-Martinez I, Martin-Lorente JL, Guarner-Argente C, Masiques ML, Vila-Miravet V, Garcia-Puig R, Savarino E, Sanchez-Vegazo CT, Santander C, Lucendo AJ. Step-up empiric elimination diet for pediatric and adult eosinophilic esophagitis: Th e 2–4–6 study. J Allergy Clin Immunol. 2018;141(4):1365–1372. https://doi.org/10.1016/j.jaci.2017.08.038
- Moawad FJ, Cheatham JG, DeZee KJ. Meta-analysis: the safety and effi cacy of dilation in eosinophilic oesophagitis. Aliment Pharmacol Th er 2013;38:713–720. https:// doi.org/10.1111/apt.12438
- Aceves SS, Newbury RO, Chen D, et al. Resolution of remodeling in eosinophilic esophagitis correlates with epithelial response to topical corticosteroids. Allergy 2010;65:109–16. https://doi.org/10.1111/j.1398– 9995.2009.02142.x
Для цитирования :
Кайбышева В. О., Эрдес С. И., Кашин С. В., Тертычный А. С. и тд. Эозинофильный эзофагит: собственный опыт диагностики и лечения. Экспериментальная и клиническая гастроэнтерология. 2018;158(10): 92–109. DOI: 10.31146/1682-8658-ecg-158-10-92-109
Загрузить полный текст
ОГЛАВЛЕНИЯ ВЫПУСКОВ
Контакты
Submission of the manuscript is online via e-mail
ecgarticle@gmail.com or
cholerez@mail.ru
Editorial Correspondence e-mail
gastrossr@gmail.com
Publishing, Subscriptions, Sales and Advertising, Correspondence e-mail
journal@cniig.ru
Tel: +7 917 561 9505
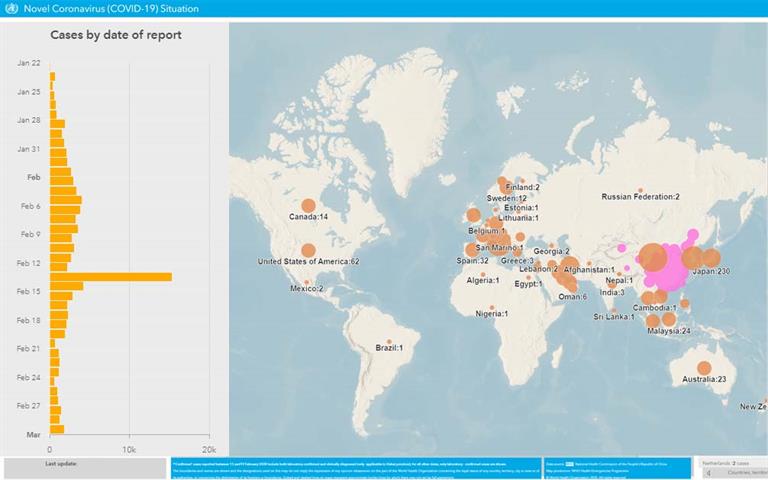
COVID-19